5 best ways to improve knee pain.
Nothing will make you feel old like a bum pair of knees. Walking can be laborious. Climbing stairs resemble climbing some snow-covered mountain. Even sitting and standing can become an Olympic event.
Maybe you want to start exercising to take off some lbs so you can save your knees. Not a bad plan until you follow a bad plan.
Following the wrong program when you have bad knees will absolutely make them worse!
Do not worry. I have you covered. Follow the steps below, and you can be on your way to moving like you used to.
These ideas work best for chronic knee pain. If you recently hurt your knee, I would not start messing with these strategies unless you have been evaluated and they are indicated for your rehab.
All of the strategies will have multiple videos to help guide you through the process. These are strategies I have used with both clients and patients to not just manage but ultimately resolve their knee pain over the last 15+ years.
I am going to go over each in more detail, but the 5 strategies are:
Remove/modify pain stimulus - this often means things like squats, lunges, running and jumping need to be tabled or altered.
Soft Tissue Mobilization (STM) - this is a $2 word for massage. Issues with your quads, IT bands, hamstrings, adductors and calfs need to be addressed.
Ankle mobility - when your ankles do not move, your knees try to move more to compensate. This is bad news for your knees.
Hip-dominant movements - this serves two purposes. It assists #1 and it builds up a part of your body that is probably weak, to begin with.
Deloaded knee-dominant movements and controlling knee valgus - all the squats and lunges and running and jumping that we took away, in the beginning, are brought back to finish your rehab.
1 - Reduce or eliminate irritating factors.
This may seem like such a 'duh' statement but you would be amazed at how many people skip this step. If a movement causes pain you must:
1️⃣ Stop doing it.
2️⃣ If you cannot stop it, you have to modify it.
3️⃣ If you cannot stop or modify, you must find the best way possible to get it done. This is not ideal and will severely delay you getting better. Sometimes, for a number of reasons, you have to perform a movement (or seven) that cause pain.
Look at these painful movements and ask, “Do I want to or do I have to do it?”
You want to? Modify or stop. Find a different way. Delegate or get help.
Have to? Find the best way and then get out of Dodge. Again, not ideal but sometimes this just has to happen.
Really pay attention to when you have the pain and where in the knee your pain is located.
⏺️ Do you have pain first thing in the morning, midday or at night? When is the pain the worst?
⏺️ Do you have pain going up or down stairs?
⏺️ Is there pain during movements or do you feel pain after doing movements?
⏺️ Is the pain on the inside of the knee (closer to the other knee), outside of the knee, over the kneecap or behind the knee?
⏺️ Does the knee feel like it swells up at all?
The more attention you can pay to these items, the better idea we will have to what is going on, what is safe to do, what to avoid and how to progress moving forward.
2 - Soft tissue mobilization.
Soft tissue mobilization (STM) is a $2 word for massage. They are similar enough, however, STM is typically more uncomfortable. There is no gently flowing water, you often start sweating from doing it and sometimes you see bright lights when you hit certain spots.
When it comes to STM, keep this idea in mind: THE MORE IT HURTS, THE MORE YOU NEED TO DO IT! This is a different rule than when you are feeling some pain during exercise.
In many cases, the tightness you feel in muscles may not be due to tightness, but chronically overstretched muscles. You can read about it at Stop stretching your tight muscles.
The knee is a fun joint that is often picked on by the hip and the ankle, but for different reasons. These will be discussed more below.
I have discussed ankle mobility in a previous post, but today we will look at some STM for the calf muscles. One of the calf muscles crosses the knee joint so it does have some impact on knee motion. But, tightness in the ankle joint is more problematic when it comes to knee pain.
Another culprit with knee pain is the IT band. The dreaded IT band. If you have ever had some STM on the ITB or used a foam roller on it, you know how amazing this is. When tight, the ITB has the potential to impact kneecap tracking. This is not a good thing.
Remember, the more it hurts, the more you need to do it. Try these to get started.
Foam roll calf - When setting up on the roller, put only one leg on at a time. This allows you to rotate the leg which allows you to hit the entire calf. Putting both feet on at the same time limits your ability to adequately target the calf muscles.
Foam roll IT band - Start out on your side with the bottom leg on the roller and the top leg crossed over in front. You will be rolling the outside part of the leg. DO NOT: 1. roll over the knee joint. This is not helpful 2. roll over the greater trochanter.
Foam roll thigh - Set up on top of the foam roller with one leg on and one leg off. This allows you to rotate from side-to-side which hits all parts of the muscle. This is not possible when both legs are on the roller. Stay above the knee joint and roll as far up the thigh as you can.
3 - Ankle mobility.
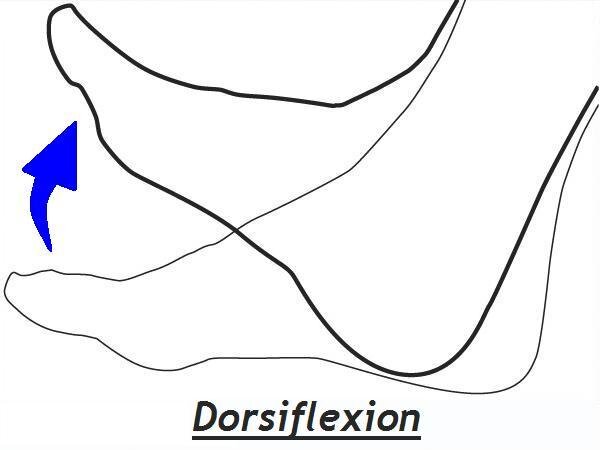
NERD ALERT! I won't go full-blown nerd on you, but a little anatomy is necessary to appreciate the relationship between the ankle and the knee. We need ankle dorsiflexion (DF) to walk and run normally. Think about bringing your foot up towards your body without taking your heel off the ground.
Another way we get DF is the lower leg (shin bone) moving forward over the ankle and foot while running and walking. This is the one that causes the issue.
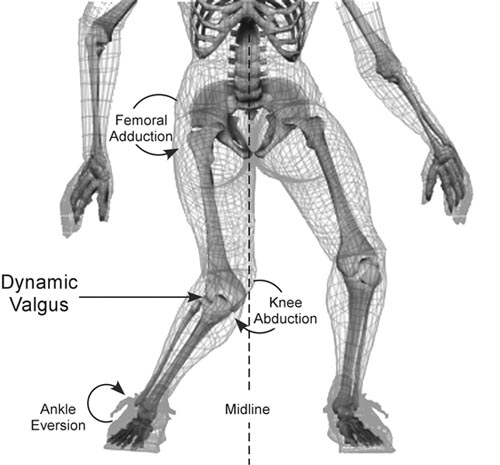
When the ankle does not move as it should, we typically lose DF. This means the lower leg cannot shift forward over the ankle like it is supposed to. When this happens, the lower leg moves towards the inside of the foot, causing the arch to collapse and the knee to collapse in towards the other knee.
This is bad news. You see, the knee is a hinge joint (for the most part). It bends and it straightens. Moving in towards the other knee stresses the joint, especially the medial (inside) of the knee.
That was bad but it gets even worse. If you keep up that movement pattern for a while (you will have to do this motion for some time before you have pain), your brain starts to treat this movement as a NORMAL movement.
So, even if you correct your ankle mobility, your knee and ankle will still collapse in. WTF?! I know, right? So, once you improve mobility, you have to spend time refining your mechanics to truly correct the issue. More on that in a minute.
I know it sounds like a lot to do, but this is the only way to truly fix the issues. If you need any help, message me to get started.
4 - Hip-dominant exercises.
This one is a no-brainer for working around knee pain initially and to help you protect your knees in the long run.
We’ve already looked at ankle mobility and how it impacts the knee. The hip is also a big contributor to knee pain too. When hip/glute muscles are weak, the hip does not stabilize properly and the result is the knee collapsing in towards the other knee.
Yup, it is this one all over again.
Sound familiar? Yes, this is the exact same motion you see when the ankle is limited. So, if you have hip/glute weakness AND ankle issues, you are totally screwed.
In addition to strengthening the hips and glutes, we also need to look at motor control and work to improve HOW we do these exercises. It is not good enough to just put your head down and power through a bunch of hip-dominant movements. HOW you do them matters.
As a general rule, when the knees are hurting, remove knee-dominant movements (squats and lunges) and focus on hip-dominant movements (bridges and deadlifts).
Here are some great options to get started with:
Box bridges - Set up on a box or boxes that are about 12-14" high. Make sure the box is right at shoulder-blade level. Focus on squeezing the glutes to lift the hips off the ground. Try to get to a table-top position. Hold the top briefly. Slowly lower back down.
Bandwalks - Step on the band and bring the hands up to about belly button-height. Start with the feet about hip-width apart. Lean to one side and squeeze the opposite hip (DO NOT swing the leg) to move the leg out to the side. Let the leg come almost all the way back in before putting it on the ground.
KB deads from a box - Set your feet so they are on either side of the step. Set and brace your lumbar spine. Keep tension in the upper back. Hinge back through the hips. DO NOT bend your knees until the hands cross the knee joint. Grab the weight and push through the heel and hips to lift the weight.
DB RDLs - RDLs are, essentially, the top portion of the deadlift. Also, you start from the stop instead of starting each rep from the floor. The DBs will not reach the floor until all reps are completed. Once you grab a pair of weights (could be DBs or KBs), keep the upper back tight and slightly bend your knees.
All of these should be able to be performed with no increase in knee pain.
5 - Deloaded knee-dominant movements and valgus knee control
The previous 4 steps took away knee-dominant movements in an attempt to let the knees calm down a bit and work on some other contributing factors.
But, at some point, you need to try these types of movements again. So what do we do? Deload.
Deloading uses something, usually bands or pulleys, for assistance during a movement. Deloading allows you to unweight joints and ask less of the muscles during a certain movement or during a certain point in the movement.
Under the watchful eye of a skilled clinician, you can also use deloaded movements to tease out whether the pain is coming from the joint or the muscles acting on the joint.
Deloading also lets us start to correct bad habits (movement impairments). I have mentioned the knee collapsing in with both ankle mobility issues and hip/glute weakness. This where we can start to fix this.
Use the assistance as much as you need to. The goal is to have pain-free movement and improve control over the movement. I typically have my clients or patients perform shorter sets (2-6 reps) at first. The goal is not to get a great leg pump. It is to perform the movement without pain AND to improve mechanics.
Deloaded squat (pulley) - Deloading the squat helps us to determine whether any pain associated with the squat is more joint or muscle in origin. The assistance should be enough to pull you up from the bottom position. Deloading also allows you to slow the descent of the squat, which often helps manage any symptoms noted during the squat.
Deloaded lunges (band) - Deloading the lunge helps us to determine whether any pain associated with a lunging motion is more joint or muscle in origin. The assistance should be enough to pull you up from the bottom position. Deloading also allows you to slow the descent, which often helps manage any symptoms noted during the lowering phase.
Go for pain-free motion. Keep the reps low and work on controlling the knee(s).
These strategies, and a little patience, can definitely get you back to a level of function you thought were lost.
If this all seems like a lot to deal with on your own, schedule a call by clicking the link below so we can talk about what is going on and see how I can help you get back on track.
Until next time,
Dr. Tom
Related posts:
5 best strategies to manage low back pain.
5 best ways to improve shoulder pain.
Tell your doctor to go pound sand.
Stop stretching your tight muscles.
Better way to do pullthroughs?
The right way to stretch your hip flexor.